THIRD DOSE RECOMMENDED FOR TRANSPLANT PATIENTS
On August 13, 2021, The Advisory Committee on Immunization Practices (ACIP) unanimously passed a resolution recommending vaccination with an additional dose of Pfizer-BioNTech or Moderna COVID-19 mRNA vaccines for moderately and severely immunocompromised people. This included those who were recipients of solid-organ or hematopoietic stem cell transplants. Immunocompromised people should continue to wear a mask, social distance and avoid crowds in poorly ventilated indoor spaces after receiving the third dose.
One month after the 3rd dose, Receptor Binding Domain (RBD) antibodies rose to 55% in the Moderna vaccinated vs. 18% in the placebo group. There were no serious adverse events [1]. 4 weeks after a third dose of the Pfizer BNT162b2 vaccine, 68% of solid-organ transplant recipients experienced a rise in antibodies vs. 40% of placebo. There were no serious adverse events or episodes of COVID-19 [2].
What are the variants?
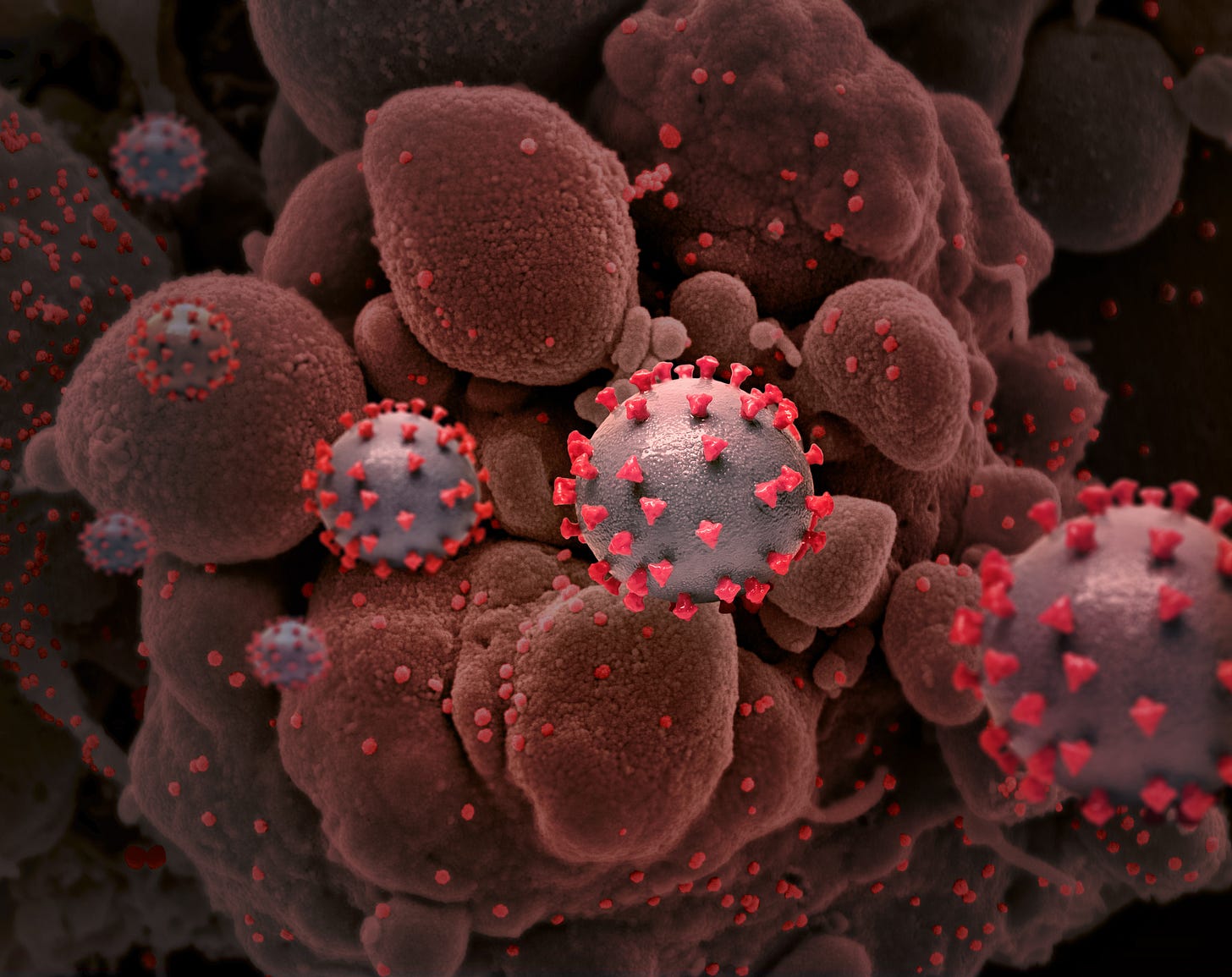
The major threat from COVID-19 is from emerging variants that either may be more infective, may be resistant to existing vaccines, or may be more lethal because of surprising new properties. Viruses mutate frequently, and if the mutation confers a survival advantage for the virus, it crowds out the original one. These variants are being closely monitored by epidemiologists:
1) Alpha from the United Kingdom (B.1.1.7);
2) Beta from South Africa (B.1.351);
3) Gamma from Japan and Brazil variant (P.1);
4) Delta (B.1.617.2 from India; and
5) Lambda variant (C.37) from South America.
All these variants, including the Lambda variant, have now been reported in the US. The Lambda variant is now the dominant mutation in Peru, Argentina, Chile, and Columbia. It may be more transmissible than the Alpha, Beta, and Gamma strains, but has yet to be compared to the Delta variant.
In the United Kingdom, the Alpha or B.1.1.7 variant was up to 70 percent more communicable than previous strains, although not more lethal. The vaccines seem effective against this variant. The Beta variant, B.1.351, from South Africa, reduced the efficacy of vaccines. The Brazil P.1 Gamma variant also reduced neutralization by the vaccine. It was reported that 73.9% of deaths carried a portion of the variant labeled G25088T. It is the Delta variant, B.1.617.2, that has dominated in the USA. That is because it is highly effective. It does respond to the vaccine, however. Its infectivity has accounted for the surge in COVID-19 cases in late summer, 2021. It is expected that the virus will continue to mutate, and may become either more infective or dangerous. Newer strains may evade vaccination and could have different pathogenesis altogether.
With respect to the Delta variant, states, where a high percentage of patients were vaccinated were compared with those where the vaccinations were relatively few. In one state with a population of 700,000 70% of patients were vaccinated, and the total cases per week were only 130. However, in a state where only 30% of the residents were vaccinated, there were 5,114 cases among the population of 300,000. The majority of cases are among the unvaccinated in both states. Among patients who were vaccinated, both the Beta and Delta variants have a variable effect on reducing antibody neutralization activity, and thus some effect on vaccine effectiveness (SOURCE: CDC).
Does immunity last?
All recipients of vaccines experience a decline in neutralizing antibodies over time. The mean titer is 235,228 in those 18-55 years old at day 119 post-second dose, 151,761 in those 56-70 years of age, and 157,946 in those over 71 years old[3].
Of 1497 healthcare workers who received the Pfizer BNT162B2 vaccine, 39 had breakthrough infections. In that group, lower neutralizing antibody titers were found at four months. Most breakthrough cases were mild. 85% of the cases were the alpha (B.1.1.7) variant [4]. Antibodies persist 8 months after infection, 6 months after the second mRNA vaccine, and 8 months after receiving a single Janssen (J&J) dose. There is decreased protection against the Beta and Gamma strains 6 months post vaccine in 50% of those given the Moderna vaccine. 50% who were protected by the vaccine against the original strain lose neutralizing antibodies 6 months later (SOURCE:CDC).
Do patients develop cellular immunity?
An article published in Nature Communications on March 19, 2020, reported that virus-specific cellular (T cell) memory can be demonstrated in SARS-COV-2 virus patients and their close contacts. The close contacts gain immunity despite never exhibiting a detectable infection [5]. This has been confirmed by additional studies. Post-infection assays of up to 317 days show that memory cells are long-lasting after infection. This should also hold for patients who are vaccinated. SARS-CoV-2-specific T cell memory is sustained in COVID-19 convalescent patients for 10 months and is associated with the successful development of stem cell-like memory T cells [6].
Should children returning to school wear a mask?
Children under 12 are currently ineligible for a vaccination although studies are exploring the safety and effectiveness of vaccinating this population. A Duke study of 7,000 children and adults who acquired COVID-19 found that there was a low rate of transmission of only 363 additional children in an environment where all wore masks (https://www.nytimes.com/2021/08/10/opinion/covid-schools-masks.html).
Should elderly persons, health care workers, nursing home residents, and those with chronic diseases receive a booster dose?
A recent study demonstrated that giving a booster vaccination 6 months after duo-vaccinations restored neutralizing antibodies in two weeks [7]. Britain, Germany, and Israel are all offering the third COVID-19 vaccine to vulnerable patients. This includes persons over 50 years of age. They are also giving booster vaccines to health care workers and care-home staff. The Advisory Committee for Immunological Practices (ACIP) will take up this issue in the coming months. The vaccines are being considered for the elderly, those who are vulnerable, and also for health care workers. A consideration with health care personnel is the heightened need to prevent even mild or asymptomatic infections in order to mitigate the risk of spread to high-risk patients.
Should a vaccine be mandated?
Health care environments such as Houston Methodist Hospital, as well as our clinical practice, are requiring vaccines. Many businesses can and will require that their patrons be vaccinated, particularly when they must congregate in a crowded environment. There are instances where a vaccine may not be warranted, i.e. those with high neutralizing antibodies, or those who have had a severe vaccination reaction. Although there are those who feel that the imposition of a government rule that individuals receive any vaccine infringes on personal rights, there is also the concern that an individual who refuses a vaccination violates the rights of others by passing along a dangerous infection. The precedents for a mandate are polio, required by each state, and smallpox. The Supreme Court of 1905 upheld that the government had the authority to reasonably infringe upon personal freedoms during a public health crisis, requiring individuals to get the smallpox vaccine or pay a fine (https://www.history.com/news/smallpox-vaccine-supreme-court). The smallpox vaccine completely eradicated a disease that plagued civilization for 400 years. Two alternatives to a mandate are that those refusing to receive a vaccine either isolate from the vulnerable or incur liability if it can be demonstrated they caused an infection. A far more favorable alternative is that a major effort is made to educate all individuals that the vaccines are safe, protect those receiving them, and as well those with whom they are in contact.
REFERENCES
[1] Hall VG, Ferreira VH, Ku T, Ierullo M, Majchrzak-Kita B, Chaparro C, et al. Randomized Trial of a Third Dose of mRNA-1273 Vaccine in Transplant Recipients. N Engl J Med. 2021.
[2] Kamar N, Abravanel F, Marion O, Couat C, Izopet J, Del Bello A. Three Doses of an mRNA Covid-19 Vaccine in Solid-Organ Transplant Recipients. N Engl J Med. 2021;385(7):661-2.
[3] Widge AT, Rouphael NG, Jackson LA, Anderson EJ, Roberts PC, Makhene M, et al. Durability of Responses after SARS-CoV-2 mRNA-1273 Vaccination. N Engl J Med. 2021;384(1):80-2.
[4] Bergwerk M, Gonen T, Lustig Y, Amit S, Lipsitch M, Cohen C, et al. Covid-19 Breakthrough Infections in Vaccinated Health Care Workers. N Engl J Med. 2021.
[5] Wang Z, Yang X, Zhong J, Zhou Y, Tang Z, Zhou H, et al. Exposure to SARS-CoV-2 generates T-cell memory in the absence of a detectable viral infection. Nature Communications. 2021;12(1):1724.
[6] Jung JH, Rha M-S, Sa M, Choi HK, Jeon JH, Seok H, et al. SARS-CoV-2-specific T cell memory is sustained in COVID-19 convalescent patients for 10 months with successful development of stem cell-like memory T cells. Nature Communications. 2021;12(1):4043.
[7] Wu K, Choi A, Koch M, Ma L, Hill A, Nunna N, et al. Preliminary Analysis of Safety and Immunogenicity of a SARS-CoV-2 Variant Vaccine Booster. medRxiv. 2021:2021.05.05.21256716.